Blog

Article
What Is Endometriosis?
5 min read
The first question most people ask me when I mention endometriosis is ‘what is that?’. And yet, 1 in 10 people assigned female at birth in the UK have it – a prevalence similar to type 2 diabetes (which most people have heard of) (1), (2). So, what’s going on here? And what is endometriosis?
Endometriosis is the presence of tissue resembling the lining of the womb (uterus) found in places outside the uterus (3). This is most commonly within the reproductive organs – often the ovaries – or further afield, affecting the bowel and bladder. The problem is that the tissue responds to the hormones of the menstrual cycle, especially oestrogen, (as does the lining of the uterus normally), resulting in cyclical changes. Long term, this can also lead to inflammation and scarring and is associated with chronic pain and infertility (4).
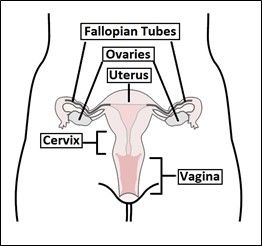
Anatomy of the uterus (5)
I know this part can be confusing, so I have added a diagram of the normal anatomy of the uterus to try and clarify this. The uterus (or womb) is shown in the middle, with the fallopian tubes on either side and then the ovaries. The lining of the uterus sheds each month during menstruation (your period). Endometriosis occurs when cells similar to this lining are found elsewhere in the body (often in the ovaries).
Why does this happen?
The reason why this happens is debated and not properly understood – I won’t bore you with the details of the theories behind it. But the most common proposal is that menstrual blood travels backwards through the fallopian tubes (instead of its normal path out the vagina) (6). Although this is the most widely accepted theory, it isn’t without its flaws. There are a lot of things about endometriosis which aren’t known, and this doesn’t help the people who suffer from it.
What are the symptoms?
This leads us on to the symptoms of endometriosis. According to the NHS website, the main symptoms are:
- Pelvic pain (pain in the lower tummy and back)
- Period pain, which is so severe that it affects everyday life
- Pain during or after sex
- Pain when going to the toilet during your period (either while peeing or pooing)
- Feeling sick, constipation, diarrhoea or blood in your pee during your period (7)
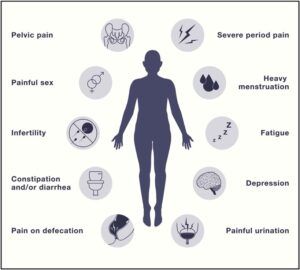
These can be alongside problems with fertility, but this is not always the case. Endometriosis often influences mental health, which can lead to anxiety and depression. There are many other less common symptoms too. Below is a summary of the ways in which endometriosis can present. If you think this could apply to you, please visit your GP for a consultation. These symptoms are not normal and, although not perfect, there are treatments available!
Symptoms of endometriosis (3)
How is it diagnosed?
The ‘gold standard’ for diagnosis of endometriosis is a surgical procedure called a laparoscopy (keyhole surgery – using small holes in the lower tummy to access the reproductive organs) (8). This is to try and view the endometriosis tissue and can be with or without taking a biopsy (sample) of the suspected lesions. This is obviously not very convenient! Patients need a GP referral to a gynaecologist to have this procedure, but it is at this point when endometriosis can either be definitively diagnosed or ruled out. There are some imaging techniques (scans) which can help with diagnosis which are improving, but aren’t perfect. This is why the keyhole surgery is required to diagnose the condition with certainty.
To make matters worse, the time taken from symptoms starting to diagnosis is extremely long – at 8 years in the UK and 8.5 years in Scotland (9). This was actually the topic of my dissertation and so I will go into some of the reasons behind this lengthy time in a future blog post. Although there is no cure for endometriosis, patients often report feeling a great sense of relief at finally getting a diagnosis. Understanding what is causing these symptoms often helps patients, who have probably been suffering for many years and never understood why.
What are the treatments?
Endometriosis, once diagnosed, often requires lifelong management. After diagnosis, the first line treatment is using contraceptives – most commonly the contraceptive pill (8). The reason for this is to try and stop the endometriotic lesions responding to oestrogen. There are also certain medications which can be given to help with the pain, but it is generally recognised that hormonal treatment will have the greatest benefit.
In more complicated cases, the lesions can be surgically removed to try and provide some relief for the patient, but this isn’t a cure. It can be even more complicated if the patient is hoping to get pregnant (as fertility problems can often result in a diagnosis). In this case, surgical management is often first line (8). Treatment of endometriosis is complicated and depends on a lot of different factors.
What are the effects of endometriosis?
The effect that endometriosis has on people’s lives is clear. It’s not hard to imagine that any (or all) of the symptoms listed above might make for a lower quality of life. These symptoms are often described as a cycle – pain and tiredness can lead to psychological symptoms such as depression and anxiety, which then leads to an increase in physical symptoms – and so on (10). Furthermore, the long wait for a diagnosis (and for treatment to start) can leave patients suffering with no explanation for their symptoms. Patients often describe a feeling that no one believes them during this time (11). A lack of general awareness about endometriosis (and sometimes embarrassment of their symptoms) can prevent people from speaking about how they are feeling to friends and family.
But, I think this is (slowly) improving. Endometriosis awareness month happens each March and will hopefully do its job in increasing awareness (12). In popular culture I have noticed an increase in open discussion of the condition. Molly Mae has talked about her experience of endometriosis on YouTube and she shows how small her scars are from surgeries. With such a big following, she will likely encourage a lot of people with symptoms to seek help, and maybe make people less scared of having the diagnostic surgery.
Molly Mae: My life with endometriosis
In BBC’s recent TV adaptation of Sally Rooney’s book, ‘Conversations with Friends’, we can see a very honest depiction of endometriosis. Francis Flynn experiences debilitating pain and heavy periods before receiving her diagnosis. When the doctor asks her if she’s heard of endometriosis, she shakes her head.
Conversations with friends
I hope I have helped to explain to you what endometriosis is and that you will feel able to speak to friends and family about it, as well as know whether your own period symptoms are normal or whether something could be wrong. See you for the next blog post!
Some links for further reading:
https://www.endometriosis-uk.org
https://www.nhs.uk/conditions/endometriosis/
References
- Scottish Government. Women’s Health Plan 2021.
- Horne AW, Saunders PTK, Abokhrais IM, Hogg L. Top ten endometriosis research priorities in the UK and Ireland. The Lancet. 2017;389(10085):2191-2.
- Saunders PTK, Horne AW. Endometriosis: Etiology, pathobiology, and therapeutic prospects. Cell. 2021;184(11):2807-24.
- Shafrir AL, Farland LV, Shah DK, Harris HR, Kvaskoff M, Zondervan K, et al. Risk for and consequences of endometriosis: A critical epidemiologic review. Best Pract Res Clin Obstet Gynaecol. 2018;51:1-15.
- Thompson L. The uterus 2019 [Available from: https://teachmeanatomy.info/pelvis/female-reproductive-tract/uterus/.
- Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. The Lancet. 2021;397(10276):839-52.
- NHS. Overview: Endometriosis 2019 [Available from: https://www.nhs.uk/conditions/endometriosis/.
- NICE. Endometriosis: diagnosis and management 2017 [Available from: https://www.nice.org.uk/guidance/ng73/resources/endometriosis-diagnosis-and-management-pdf-1837632548293.
- Endometriosis APPG ao. Endometriosis in the UK: time for change. 2020.
- Lagana AS, La Rosa VL, Rapisarda AMC, Valenti G, Sapia F, Chiofalo B, et al. Anxiety and depression in patients with endometriosis: impact and management challenges. Int J Womens Health. 2017;9:323-30.
- Rea T, Giampaolino P, Simeone S, Pucciarelli G, Alvaro R, Guillari A. Living with endometriosis: a phenomenological study. Int J Qual Stud Health Well-being. 2020;15(1):1822621.
- EndometriosisUK. Endometriosis awareness month [Available from: https://www.endometriosis-uk.org/blog/endometriosis-awareness-month-launches-tackle-fact-54-don’t-know-about-endometriosis.
Images
- Anatomy of the uterus: https://teachmeanatomy.info/pelvis/female-reproductive-tract/uterus/
- Symptoms of endometriosis: https://doi.org/10.1016/j.cell.2021.04.041
- Molly Mae – my life with endometriosis: https://www.youtube.com/watch?v=ivsvqKR3VxU
- Conversations with friends on BBC iPlayer: https://www.bbc.co.uk/iplayer/episode/p0c38bwt/conversations-with-friends-series-1-episode-11